What medicines can help control my asthma?

When you are diagnosed with asthma, your healthcare professional will start you on a treatment plan to help control your symptoms. Usually, with the right medicines, you should have very few or no asthma symptoms during the day and not have asthma attacks. If you're using your reliever inhaler more than three times a week or waking up at night one or more times a week because of asthma, it might mean your asthma isn’t well controlled.
Having the right medicines means your asthma won’t interfere with your daily life (including exercise), and your breathing tests (peak flow and spirometry) will be normal.
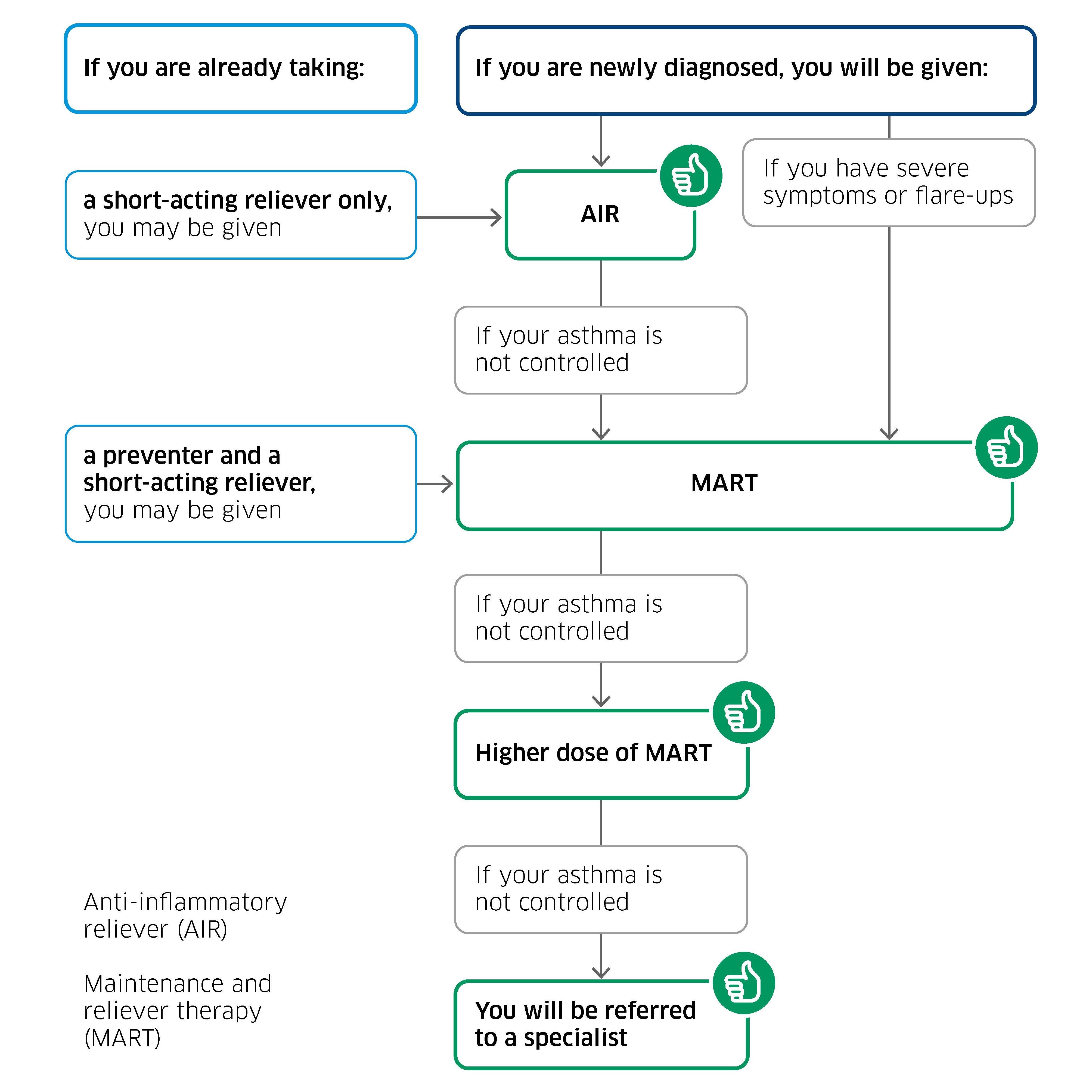
It can sometimes take time to find the right medicines for you. Your healthcare professional may have to try a few different inhalers and medicines to get your asthma under control.
Using your blue inhaler too much can be harmful. In April 2025, the Medicines and Healthcare Regulatory Agency (MHRA) reminded people that overusing a short-acting beta agonist (SABA) inhaler – often called a blue reliever inhaler – can lead to serious asthma attacks and even death. This can happen even if you’re also using a regular preventer inhaler.
If you’re using your blue inhaler more than twice a week or your asthma is getting worse, speak to your healthcare professional. They may need to change your treatment.
You might be offered a new medicine at your yearly asthma check-up or after an asthma attack to help keep your asthma under control.
Asthma medicines usually come as inhalers, and there are two main types: preventers and relievers.
Preventers (like inhaled corticosteroids) help stop symptoms from happening. Relievers (such as short-acting beta agonists or SABAs) work quickly to ease symptoms when they happen. Some inhalers contain both types of medicine. Your healthcare professional will help you find the treatment that works best for you.
Your healthcare professional may consider trying you on other medicines to help control your asthma. These are called add-on treatments and may include some of the medicines in the table below. They are used alongside your regular treatment and should not be the first option.
Other asthma medicines
| Type of medicine | How it helps |
| Leukotriene receptor antagonists
These are preventer tablets, for example montelukast. They don’t contain steroids.
|
These work by blocking one of the chemicals that is released when you come into contact with an asthma trigger. |
| Long-acting anti-muscarinic receptor antagonists
These inhaled medicines can be given in a separate inhaler, or in a single combination inhaler. An example of this is tiotropium. They can only be used as a preventer.
|
They work by providing a long-acting dilation of the airways, to allow better airway entry to your lungs. |
Recommendation based on the research evidence
You should not need long-term steroid tablets to control your asthma symptoms. There are other options for treating asthma that should be considered by a hospital specialist before long-term steroids, so you should discuss a referral to hospital with your healthcare professional. A few people with asthma may require long-term steroid tablets, after all other treatments have been tried.
Recommendation based on the research evidence
If your asthma isn’t under control, it’s important to figure out why before changing your medicines. There are many possible reasons, including:
- other diagnoses or other conditions. Sometimes, other health conditions like allergies, acid reflux (heartburn) or sinus infections can make asthma worse. Your healthcare professional may check for these
- not taking medicines as prescribed. If you find it difficult to take your medicines regularly or correctly, your asthma might not improve. This could be because of forgetfulness, side effects, or misunderstanding the instructions
- inhaler technique. Using your inhaler the wrong way can stop the medicine reaching your lungs. Your healthcare professional can show you how to use it correctly and you can watch videos on how to use it
- smoking or vaping. Smoking, even breathing in second-hand smoke, or vaping can irritate your lungs and worsen asthma
- exposure at work (occupational asthma). Breathing in fumes, dust, or chemicals at work can trigger asthma symptoms
- stress and mental health. Anxiety, depression, or stressful situations can affect how well you manage your asthma
- seasonal changes. Allergies during certain times of the year, like spring or autumn, can worsen asthma
- environmental factors. Things like air pollution, indoor mould, or pet dander might be triggers
- Having a high weight makes it harder for you to respond well to the asthma treatments. If you are overweight or obese, you should try to reach a healthy weight as part of your asthma treatment plan.
Addressing these issues can help control your asthma without needing extra medicines.
Recommendation based on the research evidence
If you are taking a moderate dose of MART, your healthcare professional may suggest a breath test or a blood test. These tests can show how much inflammation is in your airways. It might mean:
- you aren’t taking your medication regularly
- you might need a higher dose of your usual inhaler(s)
- you might benefit from an additional medicine (see Asthma medicines table above)
- you might benefit from being referred to hospital for ‘biologic’ therapy (a type of medicine made from living cells). It helps asthma by targeting the parts of the immune system that cause inflammation.
Recommendation based on the research evidence
After starting or changing your asthma medicines, you should see your healthcare professional again in 8 to 12 weeks. This check-up is important to see if:
- your symptoms have improved
- your asthma is under control
- any further adjustments are needed.
Regular follow-ups help make sure your treatment plan is right for you.
If your asthma is poorly controlled, you may be referred to hospital to see an asthma specialist.
The approach to decreasing your medicines will be different depending on whether you are on AIR, MART or have separate preventer and reliever inhalers.
| Type of treatment | Treatment plan |
|
Anti-inflammatory reliever (AIR)
|
If you have no symptoms, you will not need to take any inhaler regularly. You only take this inhaler when you have symptoms. |
|
Maintenance and reliever therapy (MART)
|
If you have not used your inhaler as a reliever, have few or no symptoms and have not had any asthma attacks, you should speak to your healthcare professional about reducing the regular inhaler dosage or stepping down to AIR. |
|
Separate preventer and reliever inhalers
|
If you have not used your reliever inhaler, have few or no symptoms and have not had any asthma attacks, you should speak to your healthcare professional about changing to AIR or MART. |
Recommendation based on clinical experience
At your yearly asthma review, your healthcare professional will talk to you about the benefits and risks of lowering your medicines. These include:
- checking if the treatment you are taking is up-to-date and fits the recommended treatments available
- increasing, decreasing, or changing your treatment, depending on how well your asthma is controlled
- taking steps to reduce medicines. Medicines will be reduced or stopped gradually, based on how well they worked for you and any side effects you experienced. You’ll wait at least 8 to 12 weeks after each adjustment to see how your asthma responds before making further changes
- monitoring and follow-up. You’ll discuss with your healthcare professional how to track your symptoms and check progress during this time. This may include keeping a symptom diary or using a peak flow meter, if it is part of your personal asthma management plan
- personal asthma action plan update. Your healthcare professional will update your personal asthma action plan. This plan includes:
- what medicines you should take
- how to recognise if your asthma is getting worse
- what to do in an emergency.
This step-down approach ensures you’re taking the least amount of medicine you need to keep your asthma well controlled.