Who to refer
Factors more likely to indicate the presence of colorectal cancer
- Age over 40years (risk rises aged 50 and rises sharply over 60 years)
- New symptoms rather than flare of previous symptoms
- Progressive symptoms > 4 weeks
Symptoms suggesting colorectal cancer
- Bleeding
- Repeated rectal bleeding without an obvious anal cause
- Blood mixed with the stool
- Bowel habit
- Persistent change in bowel habit especially to looser stools (more than 4 weeks)
- Mass
- Right-sided abdominal mass
- Palpable rectal mass
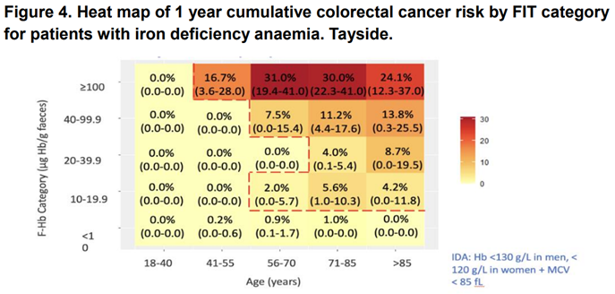
- Iron deficiency anaemia
- Unexplained iron deficiency anaemia (ie not menstrual blood loss)
- Presence of unexplained weight loss accompanied by any of:
- Rectal bleeding
- Iron deficiency anaemia
Following symptoms are low risk for colorectal cancer
- Change to constipation
- Single episode of rectal bleeding
- Abdominal pain without lower GI alarm symptoms
Who not to refer:
- Patients with other lower GI symptoms not suggestive of IBD or Colorectal Cancer
- Patients who have not had QFIT test, FBC and PR examination.
How to refer:
Refer via SCI gateway Borders Colon Service pathway:
Borders -> Borders Non-GP Locations/Providers -> Borders Colon Service -> Colonic Investigation Referral
Referrals must include:
QFIT result (QFIT value rather than QFIT result pending, or reason why it is not available)
Hb result
PR examination findings