Who to refer:
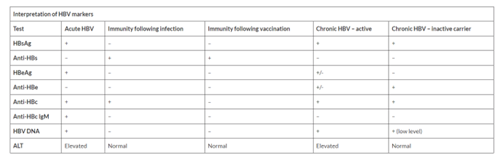
All those with chronic hepatitis B virus infection (HBsAg positive for > 6 months).
Who not to refer:
Patients who are HBsAg negative should not be referred. If the HBsAg is negative but anti-HBc is positive this indicates past infection and ongoing follow up is not required. However, these individuals may be at risk of HBV reactivation if undergoing immunosuppression. If the patient is on/being considered for immunosuppressive therapy, the hospital specialty managing the immunosuppression/chemotherapy will usually discuss the need for preventative therapy directly with HBV services.
How and where to refer:
Patients with positive HBV should be referred to the Gastroenterology team at BGH via SCI gateway as an urgent referral.
Borders General Hospital -> Gastroenterology -> Borders General referral
Patients who are also infected with HIV should be separately referred to the sexual health centre.