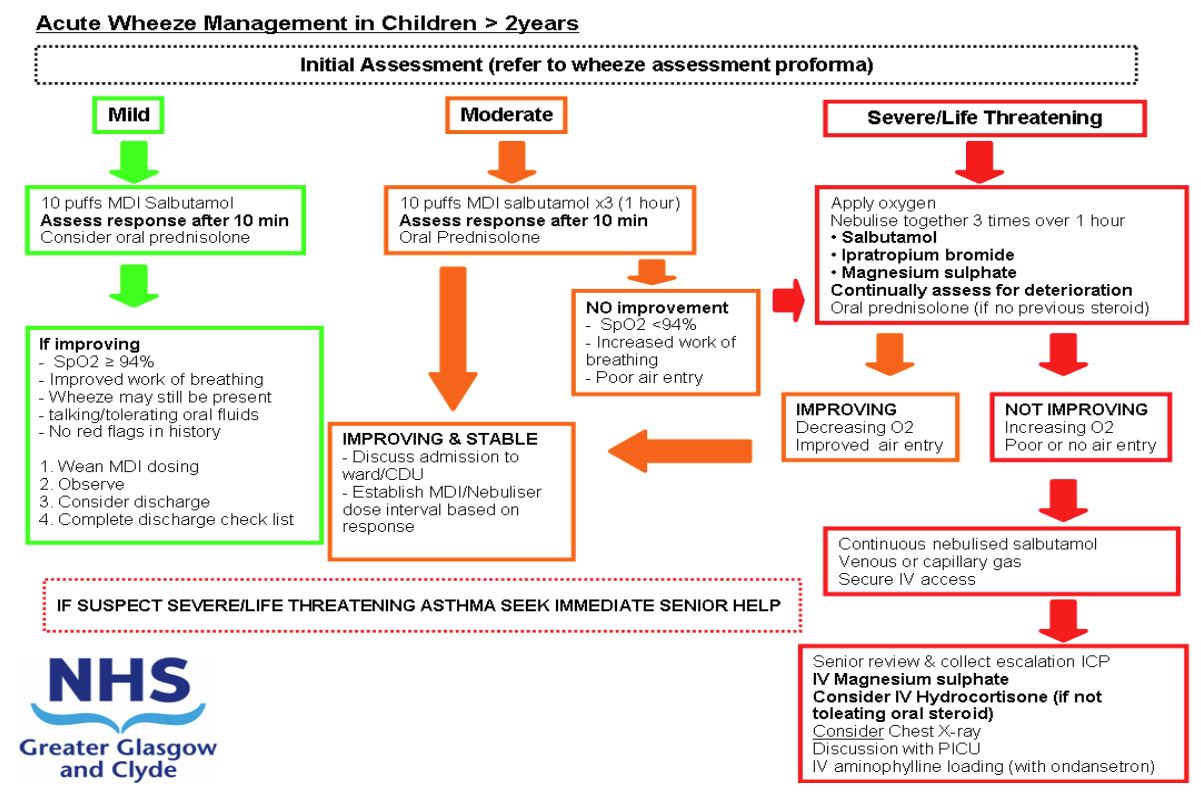
Acute wheeze in children 2 years and older: assessment and management (623)
Objectives
This guidance replaces the previous guidelines "Acute asthma in children aged between 2 and 5 years" and "Acute asthma in children > 5 years"
Separate guidance is available for Acute asthma in children aged < 2 years.
November 2023: This guidance is currently under review as it has gone beyond the standard review date. It reflects best practice at the time of authorship / last review and remains safe for use. If there are any concerns regarding the content then please consult with senior clinical staff to confirm.
|
MILD AND
|
MODERATE AND
|
|
SEVERE AND
|
LIFE THREATENING AND
|
- Has the patient previously received IV therapy for wheeze management?
- Has the patient been admitted to the PICU previously for respiratory illness?
If YES to any of the above then patient should be discussed with on call Paediatric Registrar prior to discharge.
Salbutamol MDI + Spacer – Initial therapy = 10 puffs. (100mcg per puff)
Oxygen – minimum 6 l/min via non-rebreather mask
| Prednisolone |
|
2 -4yrs 20mg OD >5yrs 40mg OD |
| Nebulised medication for Severe Wheeze | |
|
2-4yrs |
Salbutamol 2.5mg |
| >5yrs |
Salbutamol 5mg |
IV MEDICATION
(To be prescribed as per the Escalation to IV therapy care pathway)
| 1. Magnesium sulphate injection |
40mg/kg over 20 minutes (max 2gram) |
||||
|
2. Aminophylline |
|
||||
|
3. Salbutamol |
|
||||
|
- Hydrocortisone - Ondansetron |
4mg/kg QDS (max 100mg) 100micrograms/kg (max 4mg) |
- Patient maintaining saturations > 94% in air
- Tolerating 3hrly multidosing
Patients with MILD asthma at 1st assessment can be discharged after Salbutamol without being monitored for 4 hours
- Discharge Checklist Completed
- No red flag features
- If presenting with interval symptoms medication reviewed and consideration given to starting Clenil Modulite 100mcg BD
- Follow-Up arranged as below
Discharge planning - points to consider
Discharge Checklist Completed?
All the following must be completed prior to discharge
- Inhaler technique checked
- Asthma booklet given
- Watched asthma education video
- Completed 3 days prednisolone or remaining doses prescribed for home
- Salbutamol inhaler (x2) and spacer dispensed
- Wheeze plan given and explained
- Parents advised what to do in event of clinical deterioration
- Advised to attend GP within 48 hours discharge
- Chronic features and criteria for follow-up reviewed
- (Please document any follow-up requested)
- Maintaining oxygen Saturations >/= 94% air
- Tolerating 3hrly multi-dosing
- Discharge Medication prescribed
Chronic features / Interval symptoms
If any of the following features:
- 3 or more ED presentations with wheeze in 1 year
- 3 or more courses of steroids for wheeze in 1 year
- Answered yes to interval symptoms on wheeze proforma
AND not on a Preventer inhaler then prescribe Clenil modulite 100mcg BD
If already on a preventive inhaler review compliance and criteria for follow-up to assess need for hospital outpatient based follow up.
Criteria for Acute Medical Paediatric Follow Up
GP’s should be able to manage the majority of children with wheeze
Patients who have been started on a clenil inhaler should be advised to attend their G.P. in 6 weeks to assess response.
Children where there is diagnostic uncertainty or very young children (between the ages of 2 and 3) with concern about recurrent presentations then discuss Follow up planning with either the general paediatrician or senior paediatric registrar on tel: 84678.
Criteria for Respiratory Team Follow Up
Any child requiring intravenous therapy for wheeze.
Patients who have required intravenous therapy for wheeze should be monitored in hospital for at least 24 hours post the discontinuation of all intravenous therapy.
Any child where there is a concern that they have failed to respond to significant asthma treatment.
ALL RESPIRATORY REFERRALS SHOULD BE DISCUSSED WITH RESPIRATORY TEAM PRIOR TO PATIENT DISCHARGE FROM HOSPITAL.