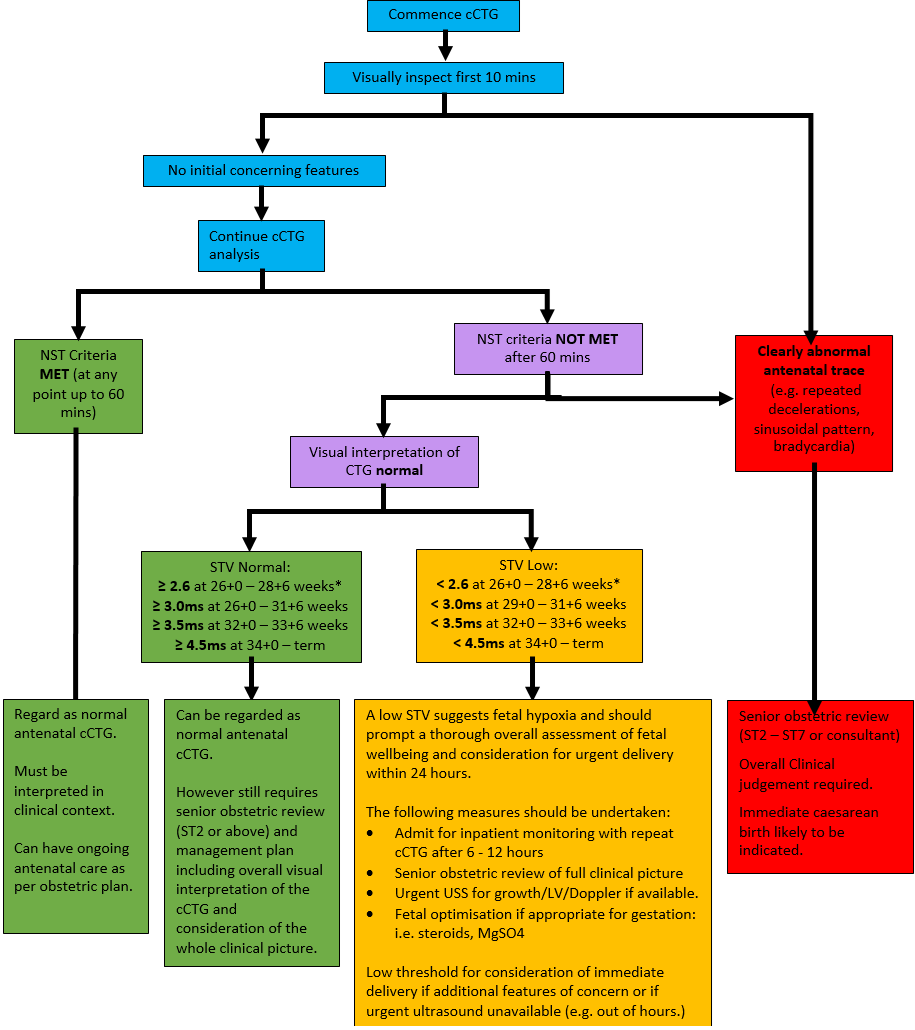
CTG is not a replacement of clinical judgement. In the presence of other associated signs or symptoms suggestive of maternal or fetal compromise, further assessment is required, even if a cCTG is deemed normal. It is also important to remember that intrapartum NICE CTG guidance is NOT applicable in the antenatal period. Dawes Redman analysis assesses fetal wellbeing based on a specific data set. Low STV is the best predictor of fetal acidaemia and risk of in utero demise. Mean STV increases as gestation advances. Typically, in healthy fetuses it increases from around 6ms at 26 weeks to 8ms at term. Considering information applied from TRUFFLE (Trial of Randomised Umbilical and Fetal Flow in Europe), if the STV falls below the threshold for the gestation, delivery should be considered due to suspected hypoxia in the fetus. If any other features of the antenatal CTG are suspected to be abnormal, such as repeated decelerations, fetal bradycardia or sinusoidal pattern, an immediate obstetric review must be sought and immediate delivery considered. NB. The cCTG analysis will flag any STV <3.0ms as abnormal however at gestations < 29+0 weeks an STV ≥ 2.6ms is acceptable as per ISUOG Practice Guideline: diagnosis and management of small-for-gestational-age fetus and fetal growth restriction.5 On Phillips Avalon CTG monitors used in NHS GGC, this is referred to as NST criteria.
When a cCTG is carried out the following outcomes are possible:
- Dawes Redman NST Criteria MET (at any point up to 60 mins): Regard this as a normal antenatal cCTG, however it is still important to look at the whole clinical picture. The patient can have ongoing antenatal care as per their obstetric plan.
- Dawes Redman NST Criteria NOT met after 60 mins but STV normal:
If on visual inspection the cCTG looks normal for the gestation AND the STV is normal for the gestation (≥ 2.6ms at 26+0 – 28+6 weeks, ≥ 3.0ms at 29+0 – 31+6 weeks, ≥ 5ms at 32+0 – 33+6 weeks or ≥ 4.5ms at 34+0 - term)5 this can also be regarded as a normal antenatal cCTG. The whole clinical picture and cCTG trace should be reviewed by a senior doctor (ST2 - ST7 or consultant).
NB The cCTG analysis will flag any STV <3.0ms as abnormal however at gestations < 29+0 weeks an STV ≥ 2.6ms is acceptable (as per ISUOG Practice Guideline: diagnosis and management of small-for-gestational-age fetus and fetal growth restriction5) and can be regarded as normal.
- Dawes Redman NST Criteria NOT met after 60 mins and STV is low: A low STV (< 2.6ms at 26+0 – 28+6 weeks, < 3.0ms at 29+0 – 31+6 weeks, < 3.5ms at 32+0 – 33+6 weeks or < 4.5ms at 34+0 - term)5 suggests fetal hypoxia and should prompt a thorough overall assessment of fetal wellbeing and consideration for urgent delivery by caesarean birth within 24 hours.
The following measures should be undertaken:
- Admit for inpatient monitoring
- Senior (ST2 – ST7 or consultant) obstetric review of full clinical picture
- Urgent USS for growth/LV/Doppler if available.
- Fetal optimisation if appropriate for gestation: i.e. steroids, MgSO4
There should be a low threshold for consideration of immediate caesarean birth if there are additional features of maternal or fetal concern or if urgent ultrasound is unavailable (e.g. out of hours). Decision to deliver a preterm infant should include discussion with the on-call consultant obstetrician.
- Clearly abnormal antenatal CTG (e.g. prolonged repeated decelerations, bradycardia, sinusoidal pattern): As soon as this is recognised there should be IMMEDIATE senior (ST2 - ST7 or consultant) obstetric review to assess the whole clinical picture including visual inspection of the cCTG. An emergency caesarean birth is likely to be indicated. Delivery of a preterm infant should always be discussed with the on-call consultant obstetrician.
It is important to bear in mind that when the criteria are not all met by 60 minutes, this DOES NOT automatically indicate that the cCTG is abnormal. It does however indicate that the computerised analysis is not certain that all the parameters are within normal limits, and the cCTG trace therefore requires careful human interpretation and particular attention paid to the STV.
See Appendix 1 for guidance on how to interpret a cCTG in a flow chart format.
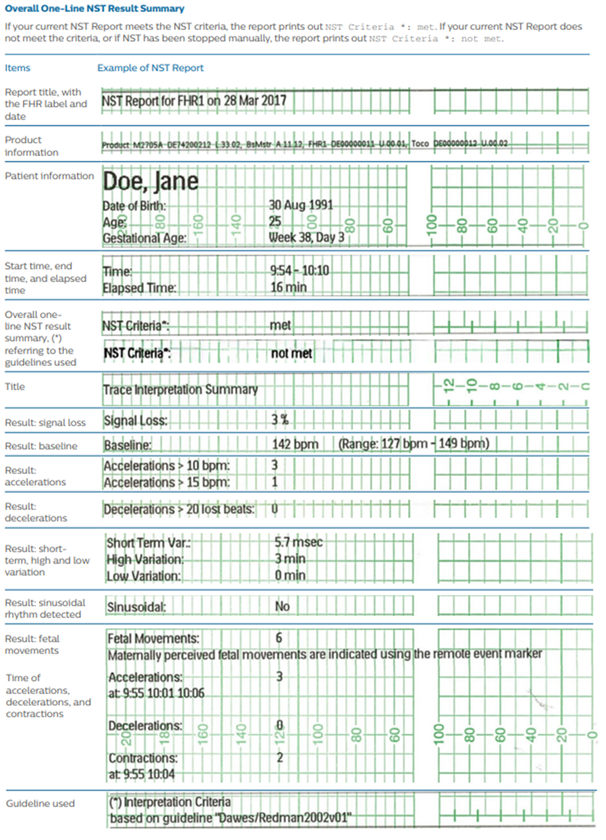
See Appendix 2 for an example report of a cCTG.