Physical health monitoring and treatment interventions for individuals who are prescribed OST and are using cocaine

An update of the physical health history and regular review of all prescribed medication is particularly important for individuals using cocaine as there is greater risk of strain on the heart from medications which prolong the QT interval. There is also an increased risk with sedative medications, both prescribed and non-prescribed, that cocaine may mask the depressant impact on the respiratory system and so increase risk of overdose.
There is evidence that participation in treatment and commencement of opioid substitution therapy (OST) can be associated with reduced cocaine use in individuals with opiate dependence also using cocaine. It would therefore not be advisable to delay OST in an attempt to stabilise cocaine use first.
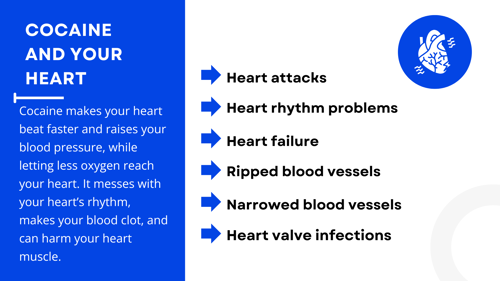
An ECG can give a helpful indication of strain on the heart and any prolongation of the QT interval. Where possible this is helpful at initiation of OST or during changes in dose. If this is not possible a balanced judgement is required as holding up vital treatment to await an ECG first may increase rather than reduce risk to health.
There is reduced risk of QT interval prolongation (adding to heart strain) and reduced respiratory depression risk with buprenorphine compared to methadone. Although there is no specific recommendation in OST choice for individuals with opiate dependence who are using cocaine, this should be taken into consideration along with other individual factors.
Individuals who start to use cocaine during OST may require an update in their risk and Red/Amber/Green (RAG) assessment and more regular support from their care manager. Consideration should be given to instalment dispensing of OST.
Cocaine use should not prevent an increase in OST if this is indicated. Stabilising on an optimal dose of OST may not only make it easier for the individual to reduce and stop using non-prescribed opiates but also other drugs such as cocaine.