The complaints handling procedure aims to provide a quick, simple and streamlined process for resolving complaints early and locally by capable, well-trained staff.
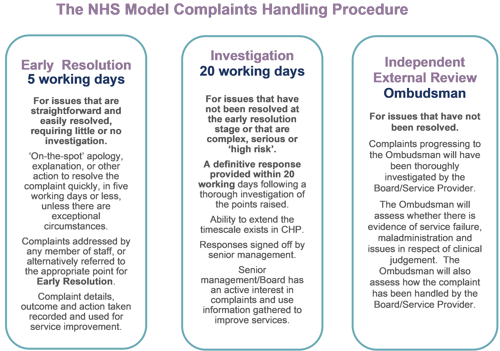
Our complaints handling procedure provides two opportunities to resolve complaints internally:
- early resolution; and
- investigation
For clarity, the term ‘early resolution’ refers to the first stage of the complaints process. It does not reflect any job description or role within NHS Borders but means seeking to resolve complaints at the initial point of contact where possible.
What to do when a complaint is received
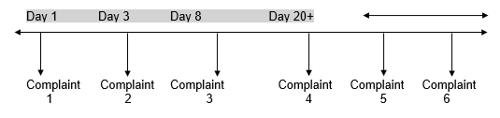
- On receiving a complaint, a decision must be made whether the issue can indeed be defined as a complaint. (see flowchart at Appendix 5) The person making the complaint may express dissatisfaction about more than one issue. This may mean one element is treated as a complaint, while directing the person to pursue another element through an alternative route.
- Once received and identified as a complaint, the details should be recorded on the complaints system.
- Next, decide whether or not the complaint is suitable for early resolution. Some complaints will need to be fully investigated before a suitable response may be give. These complaints must be handled immediately at the investigation stage.
- Where early resolution is appropriate, four key questions must be considered:
- what exactly is the person's complaint (or complaints);
- what do they want to achieve by complaining;
- can this be achieved, and if not why not; and
- can this be resolved, who can help with early resolution?
What exactly is the person’s complaint (or complaints)?
Find out the facts. It is important to be clear about exactly what the person is complaining of, more information may be required to get a full picture.
What do they want to achieve by complaining?
At the outset, clarify the outcome the person wants. Of course, they may not be clear about this, probing further may be required to find out what they want, and whether the expected outcome can be achieved. It may also be helpful to signpost people who complain to PASS at this point as advisers can often help clients think about their expectations and what is a realistic/reasonable outcome to expect.
Can I achieve this, or explain why not?
If the expected outcome can be achieved by providing an on-the-spot apology or explain why you cannot achieve it, you should do so.
The person making the complaint may expect more than can be provided, or a form of resolution that is not at all proportionate to the matter complained about. If so, you must tell them as soon as possible. An example would be where someone is so dissatisfied with their experience in ‘Accident and Emergency’ that they want the Chief Executive to be sacked.
You are likely to have to convey the decision face to face or on the telephone. If you do this, you are not required to write to the person as well, although you may choose to do so. It is important, however, to record full and accurate details of the decision reached and passed to the person, and to ensure that they understand the outcome. You must also advise them of their right to have the complaint escalated to stage 2 of the complaints procedure if they are not satisfied with the outcome at the early resolution stage.
If I cannot resolve this, who can help with early resolution?
If you cannot deal with the complaint because, for example, you are unfamiliar with the issues or area of service involved, tell the person this and pass details of the complaint to someone who can attempt to resolve it. Keep the person making the complaint informed about what has happened to their complaint and who is responsible for taking it forward.
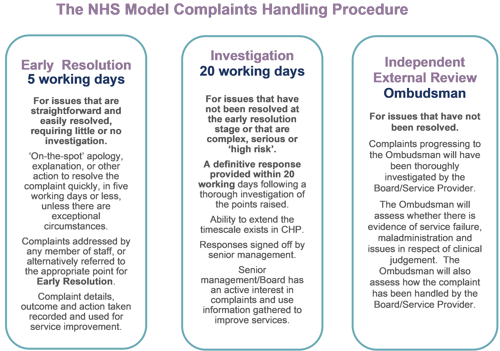
Stage one: early resolution
Early resolution aims to resolve straightforward complaints that require little or no investigation at the earliest opportunity. This should be as close to the point of service delivery as possible. Any member of staff may deal with complaints at this stage. In practice, early resolution means resolving the complaint at the first point of contact with the person making the complaint. This could mean a face-to-face discussion with the person, or it could mean asking an appropriate member of staff to deal directly with the complaint. In either case, a complaint may be settled by providing an on-the-spot apology where appropriate, or explaining why the issue occurred and, where possible, what will be done to stop this happening again.
An explanation may also be given that, as an organisation that values complaints, the information given in a complaint may be used when service standards are reviewed in the future.
Anyone can make a complaint. They may do so in writing, in person, by telephone, by email or online, or by having someone complain on their behalf. Early resolution must always be considered, regardless of how the complaint has been received.
Appendix 1 gives examples of the types of complaint which may be considered at this stage, with suggestions on how to resolve them.
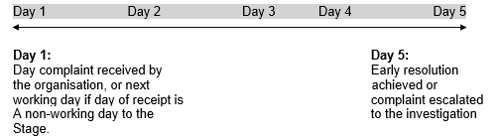
Timelines (Stage one)
Early resolution must usually be completed within five working days, although the expectation would be to resolve the complaint much sooner.
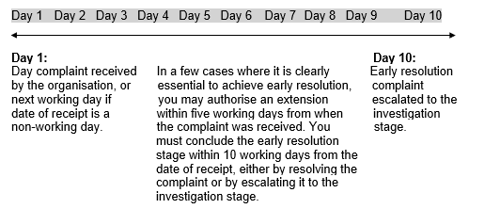
Extension to the timeline
In exceptional circumstances, where there are clear and justifiable reasons for doing so, an extension may be agreed of no more than five additional working days with the person making the complaint. This must only happen when an extension will make it more likely that the complaint will be resolved at the early resolution stage.
For example, more information may be required from other services to resolve the complaint at this stage. However, it is important to respond within the applicable time to the person making the complaint, either resolving the matter and agreeing with the person that this has been achieved, or explaining that their complaint is to be investigated.
When you ask for an extension, you must get authorisation from the appropriate senior manager, who will decide whether you need an extension to effectively resolve the complaint. Examples of when this may be appropriate include staff or contractors being temporarily unavailable. You must tell the person making the complaint about the reasons for the delay, and when they can expect your response.
Where, however, the issues are so complex, and it is clear that they cannot be resolved within an extended five day period, you should escalate the complaint directly to the investigation stage.
It is important that extensions to the timeline do not become the norm. Rather, the timeline at the early resolution stage should be extended only rarely. All attempts to resolve the complaint at this stage must take no longer than ten working days from the date you receive the complaint.
The proportion of complaints that exceed the five working days timeline at the early resolution stage will be evident from reported statistics. These statistics must go to the senior management team on a quarterly basis. Appendix 6 provides further information on timelines.
Closing the complaint at the early resolution stage
When you have informed the person making the complaint of the outcome at early resolution, you are not obliged to write to them, although you may choose to do so. You must ensure that the response to the complaint addresses all areas of responsibility explain the reasons for the decision. It is also important to keep a full and accurate record of the decision reached and given to the person. The complaint should then be closed and the complaints system updated accordingly. In closing the complaint, the date of closure is the date that the outcome of the complaint at the early resolution stage is communicated to the person making the complaint.
When to escalate to the investigation stage
A complaint must be handled at the investigation stage when:
- early resolution was tried but the person making the complaint remains dissatisfied and requests an investigation into the complaint. This may be immediately on communicating the decision at the early resolution stage or could be some time later; or
- satisfactory early resolution will not be possible as the complainant has clearly insisted that an investigation be conducted.
Complaints should be handled directly at the investigation stage, without first attempting early resolution, when:
- the issues raised are complex and require detailed investigation; or
- the complaint relates to serious, high-risk or high-profile issues.
When a complaint is closed at the early resolution stage, but is subsequently escalated to the investigation stage of the procedure, it is important that the complaint outcome is updated on the complaints system, and the complaint moved to stage 2. A new complaint should not be recorded.
It is also important to take account of the time limit for making complaints when a person asks for an investigation after early resolution has been attempted. The timescale for accepting a complaint as set out in the Regulations is within six months from the date on which the matter of the complaint comes to the person’s notice.
While attempting early resolution always take particular care to identify complaints that on fuller examination might be considered serious, high risk or high profile, as these may require particular action or raise critical issues that need senior management's direct input.
Stage two: investigation
Not all complaints are suitable for early resolution and not all complaints will be satisfactorily resolved at that stage. Complaints handled at the investigation stage of the complaints handling procedure are typically serious or complex, these require a detailed examination before a response can be given on our position. These complaints may already have been considered at the early resolution stage, or they may have been identified from the start as needing immediate investigation.
An investigation aims to establish all the facts relevant to the points made in the complaint and to give the person making the complaint a full, objective and proportionate response that represents the final position.
What to do when you receive a complaint for investigation
It is important to be clear from the start of the investigation stage exactly what you are investigating, and to ensure that both the person making the complaint and the service understand the investigation’s scope.
If this has not been considered at the early resolution stage, you should discuss and confirm these points with the person making the complaint at the outset, to establish why they are dissatisfied and whether the outcome they are looking for sounds realistic. In discussing the complaint with the person, consider three key questions:
- What specifically is the person’s complaint or complaints?
- What outcome are they looking for by complaining?
- Are the person's expectations realistic and achievable?
It may be that the person making the complaint expects more than can be provided. If so, this must be made clear to them as soon as possible.
Where possible you should also clarify what additional information you will need to investigate the complaint. The person making the complaint may need to provide more evidence to help in reaching a decision.
You should find out what the person’s preferred method of communication is, and where reasonably practicable communicate by this means.
Details of the complaint must be recorded on the system for recording complaints. Where applicable, this will be done as a continuation of the record created at early resolution. The details must be updated when the investigation ends.
If the investigation stage follows attempted early resolution, you must ensure you have all case notes and associated information considered at the early resolution stage. You must also record that this information has been obtained.
Contact with the person making the complaint at the start of the investigation
To effectively investigate a complaint, it is often necessary to have a discussion with the person making the complaint to be clear about exactly what the complaint or complaints relate to, understand what outcome the person making the complaint is looking for by complaining, and assess if these expectations are realistic and achievable. This may be by a telephone discussion or it may be appropriate to arrange a meeting between appropriate NHS staff and the person making the complaint. This will provide the opportunity to explain how the investigation will be conducted, and to manage the person’s expectations in regard to the outcomes they are looking for. Where the complainant prefers to only have contact via email or letter this can be facilitated.
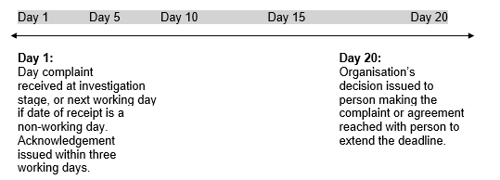
Timelines (Stage two)
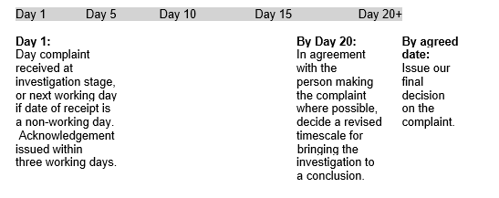
The following deadlines are set out in the Regulations for cases at the investigation stage:
- complaints must be acknowledged within three working days; and
- you should provide a full response to the complaint as soon as possible but not later than 20 working days, unless an extension is required.
Acknowledgements
The Complaints Directions set out what must be included in a written acknowledgement of a complaint, which is as follows:
- contact details of the Patient Experience Officer;
- details of the advice and support available including the PASS;
- information on the role and contact details for the SPSO;
- a statement confirming that the complaint will normally be investigated, and the report of the investigation sent to the complainant, within 20 working days or as soon as reasonably practicable; and
- a statement advising that, should it not be possible to send a report within 20 working days, the person making the complaint will be provided with an explanation as to why there is a delay and, where possible, provided with a revised timetable for the investigation.
When advising the person making the complaint about the role and contact details of the SPSO, it should also be explained that if they remain dissatisfied at the end of the complaints process, they can ask the SPSO to look at their complaint, and that further information about this will be provided with the final decision on the complaint.
When issuing the acknowledgement letter you should issue it in a format which is accessible to the person making the complaint. You should also consider including the following points, where relevant to the complaint:
- thank the person making the complaint for raising the matter;
- summarise your understanding of the complaint made and what the person making the complaint wants as an outcome (this information will be available to you from your actions at ‘What to do when you receive a complaint’ as documented above);
- where appropriate the initial response should express empathy and acknowledge the distress caused by the circumstances leading to the complaint;
- outline the proposed course of action to be taken or indicate the investigations currently being conducted, stressing the rigour and impartiality of the process;
- offer the opportunity to discuss issues either with the investigation officer, the complaints staff or, if appropriate, with a senior member of staff;
- request that a consent form is completed where necessary; (appendix 7)
- provide information on alternative dispute resolution services and other support service such as advocacy; and
- provide a copy of the ‘Public Facing Complaints Handling Procedure’ if this has not already been issued.
You may send the letter electronically, provided that the person making the complaint has consented to this in writing, and has not withdrawn their consent.
During the course of the investigation, you should, where possible ensure that the person making the complaint, and anyone involved in the matter which is the subject of the complaint, is informed of progress and given the opportunity to comment.
Meeting with the person making the complaint during the investigation
To effectively investigate the complaint, it may be necessary to arrange a meeting with the person making the complaint. Where a meeting takes place, always be mindful of the requirement to investigate complaints within 20 working days wherever possible. There is no flexibility within the Patient Rights (Scotland) Act 2011 to ‘stop the clock’ in the complaints handling process. This means that where required, meetings should always be held within 20 working days of receiving the complaint wherever possible. As a matter of good practice, where meetings between NHS staff and the person making the complaint do take place, a written record of the meeting should be completed and provided to the person making the complaint. Alternatively, and by agreement with the person making the complaint, you may provide a record of the meeting in another format, to suit their communications needs and preferences. You should discuss and agree with the person making the complaint, the timescale within which the record of the meeting will be provided.
Extension to the timeline
It is important that every effort is made to meet the timescales as failure to do so may have a detrimental effect on the person making the complaint. Not all investigations will be able to meet this deadline, however, and the Regulations allow an extension where it is necessary in order to complete the investigation. For example, some complaints are so complex that they require careful consideration and detailed investigation beyond the 20 working day limit. However, these would be the exception and you must always try to deliver a final response to a complaint within 20 working days.
If there are clear and justifiable reasons for extending the timescale, the Patient Experience Officer will set time limits on any extended investigation, as long as the person making the complaint agrees. You must keep them updated on the reason for the delay and give them a revised timescale for completion. If the person making the complaint does not agree to an extension but it is necessary and unavoidable, then senior management must consider and confirm the extension.
The reasons for an extension might include the following:
- essential accounts or statements, crucial to establishing the circumstances of the case, are needed from staff, patients or others but they cannot help because of long-term sickness or leave;
- you cannot obtain further essential information within normal timescales;
- operations are disrupted by unforeseen or unavoidable operational circumstances, for example industrial action or severe weather conditions; or
- the person making the complaint has agreed to mediation as a potential route for resolution.
These are only a few examples, and the matter must be judged individually in relation to each complaint.
As with complaints considered at the early resolution stage, the proportion of complaints that exceed the 20-day limit will be evident from reported statistics.
If you are handling a complaint spanning health and social care services and the health aspects have been resolved but the social care aspects require an extension to continue investigation, you must tell the person that you are not yet in a position to respond to all aspects of the complaint and tell them when you will do so. Appendix 6 provides further information on timelines.
Mediation
Some complex complaints, or complaints where the person making the complaint and other interested parties have become entrenched in their position, may require a different approach to resolution. Where appropriate, you may consider using services such as mediation or conciliation, using suitably trained and qualified mediators to try to resolve the matter and to reduce the risk of the complaint escalating further.
Mediation will help both parties to understand what has caused the complaint, and so is more likely to lead to mutually satisfactory solutions. It can be particularly helpful in the context of complaints about primary care providers, and the Directions set out that Boards must provide alternative dispute resolution services in these circumstances, if both the person making a complaint about a primary care provider, and the person subject to the complaint, agree that it should be provided.
If you and the person making the complaint agree to mediation an extension to the investigation period is likely to be necessary and, revised timescales should be agreed.
Closing the complaint at the investigation stage
In terms of best practice, for relevant NHS bodies, the complaints process should always be completed by the Patient Experience Manager (or someone authorised to act on his or her behalf) reviewing the case. They must ensure that all necessary investigations and actions have been taken. For other health service providers this will be the Patient Experience Officer or a senior officer nominated to perform this review. Where the complaint involves clinical issues, the draft findings and response should be shared with the relevant clinicians to ensure the factual accuracy of any clinical references. Where this is appropriate the relevant clinicians should always have regard to the timescales within which the decision should be issued.
You must let the person making the complaint know the outcome of the investigation, in writing, and also, if applicable, by their preferred alternative method of contact. Response to the complaint must address all areas NHS Borders are responsible for and explain the reasons for our decision. You must record the decision, and details of how it was communicated to the person making the complaint, on the system for recording complaints. In accordance with the Complaints Directions, the report must include the conclusions of the investigation and information about any remedial action taken or proposed as a consequence of the complaint.
The report must be signed by an appropriately senior person. You may send this report electronically, provided that the person making the complaint has consented to this in writing, and has not withdrawn their consent.
The quality of the report is very important and in terms of best practice should:
- be clear and easy to understand, written in a way that is person-centred and non-confrontational;
- avoid technical terms, but where these must be used to describe a situation, events or condition, an explanation of the term should be provided;
- address all the issues raised and demonstrate that each element has been fully and fairly investigated;
- include an apology where things have gone wrong;
- highlight any area of disagreement and explain why no further action can be taken;
- indicate that a named member of staff is available to clarify any aspect of the letter; and
- indicate that if they are not satisfied with the outcome of the local process, they may seek a review by the Scottish Public Services Ombudsman. Details of how to contact the Ombudsman’s office should be included in the response.
Meetings and post decision correspondence with the person making the complaint
As previously noted, it is often appropriate to meet with the person making the complaint at the outset of the investigation in order to fully understand the complaint, what the person making the complaint wants to achieve by complaining, and to explain how the complaint will be handled.
A request for a meeting may also be received once the person making the complaint receives the decision on their complaint. The circumstances in which a meeting may be requested after the decision letter has been received include:
- The person requests further explanation or clarification of the decision or suggests a misunderstanding of the complaint in terms of the response.
- The person does not agree with some, or all of the response in terms of the investigation’s findings or conclusions or with the decision on the complaint.
- A combination of points 1 and 2 above, where for example the person suggests the complaint has not been fully understood, and the decision is erroneous even in the aspects that have been properly considered.
It should be made clear that such a meeting is for explanation only and not a reinvestigation or reopening of the complaint.