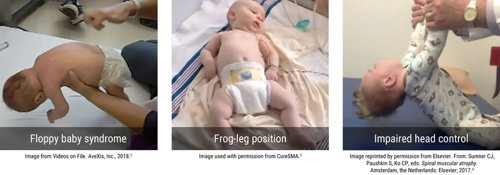
Babies who are hypotonic may present to health visitors, GPs, paediatric physiotherapists, neonatal clinic, neurology clinic, community child health clinic or the Paediatric Assessment Unit. They may present with other health issues and hypotonia is noted as part of that assessment.
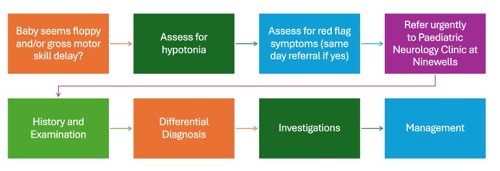
True hypotonia is uncommon in babies and is almost always the result of a significant underlying health issue. Some of these medical conditions, such as Spinal Muscular Atrophy, are treatable and earlier treatment is associated with improved outcomes. For this reason, floppy babies need to be assessed promptly by an experienced paediatrician. In Tayside, hypotonic infants should be referred urgently to the Paediatric Neurology team, as per the pathway below.