Fibromyalgia

Referring to rheumatology
Refer to rheumatology only if there are features other than pain that raise suspicion of an inflammatory muscle or joint condition. The rheumatology team are unlikely to be able to offer much beyond confirmation of a diagnosis of fibromyalgia; management is outlined below.
Background
Fibromyalgia is common with a prevalence of 2% in the general population. However, it often takes >2 years for a diagnosis to be made. Referral to specialists and multiple investigations result in high healthcare costs. Due to the constellation of symptoms its impact can be severe. It is associated with poor quality of life and often promotes physical inactivity, social withdrawal, and psychological distress.
Diagnosis
There are no specific diagnostic tests for fibromyalgia.
It is appropriate to exclude other causes of fatigue and myalgia such as thyroid dysfunction and vitamin D deficiency. It is unusual for fibromyalgia to present in a similar fashion to inflammatory rheumatological conditions but it may be reasonable to check CRP if an inflammatory condition is suspected.
The American College of Rheumatology Diagnostic Criteria suggest a diagnosis is made when all of the following criteria are met:
- Widespread pain
- Generalized pain, defined as pain in at least 4 of 5 regions (left and right upper quadrants, left and right lower quadrants and spine), is present.
- Symptoms have been present at a similar level for at least 3 months.
- A diagnosis of fibromyalgia is valid irrespective of other diagnoses. A diagnosis of fibromyalgia does not exclude the presence of other clinically important illnesses.
The symptom severity index and widespread pain index is a useful guide. Other symptoms include:
- Sleep disturbance/non restorative sleep
- Headaches
- Impaired concentration/poor memory
- Anxiety and depression
- Non-anatomical paraesthesia
- Irritable bowel syndrome
- Irritable bladder
- Hypersensitivity
- Non-cardiac chest pain.
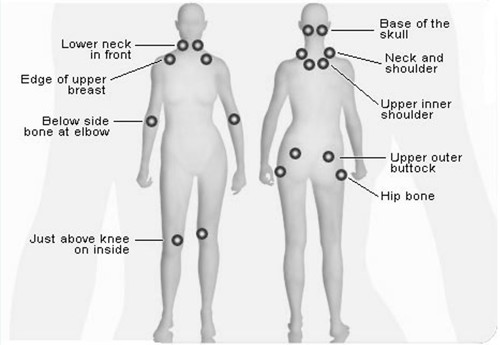
Although NOT part of the diagnostic criteria, it is recognised that patients with fibromyalgia are often tender in particular locations:
Management summary
- Explanation of the diagnosis to the patient with written education given – having a name for their condition is helpful for patients
- Emphasis on the fact that management is long term and multi-factorial and that medication is unlikely to fully resolve symptoms
- Physical therapy with graded physical exercise, either via physiotherapy or referral to a local fitness programme
- Alternative therapies can be explored, although most of these are not available through NHS referral
- For analgesic options refer to local formulary for chronic pain management
- Referral for psychological assessment and therapy for those with significant depression, anxiety or poor coping strategies
- For referral to pain service, please check local chronic pain management pathways.
Resources
- Versus Arthritis booklet on fibromyalgia
- Pain Association Scotland is a charity which organises community based group education and self-management programmes for patients with chronic pain
- Fibromyalgia Action UK is a charity which offers patient information and online support
- The European League Against Rheumatism (EULAR) recommendations for the management of fibromyalgia