Allergy
- Confirm no allergy to skin preparation or products in line
Bleeding
- Check platelet count and coagulation status: consider benefits of optimising
- Consider stopping anticoagulant and/or antiplatelet therapy – balance of risks will depend on the urgency of CVC and risks of stopping therapy
Task fixation
- Ensure adequate monitoring: ECG, SpO2, BP as minimum
- Ensure there is a colleague assisting at the bed space during line insertion
- Patient observation/Monitoring/Procedural tasks including “WIRE OUT” response
Sterility and PPE
- Hat, mask, eye protection, sterile gloves and gown
- Large fenestrated drape + / - additional sterile drapes
- Ideally a fresh, unused site
- 2% chlorhexidine in 70% Isopropyl alcohol prepping from insertion point outwards; allowed to dry
- Clean blood from site post insertion and apply transparent occlusive dressing
Air embolism
- Patient positioning
- Head down tilt for subclavian or internal jugular lines
- Supine for femoral lines
- All ports should be flushed before insertion
- All but the distal port should be clamped or closed with a sterile bung
- Use self-sealing bungs on all ports from time of insertion
- Avoid using 3-way taps where possible. If used, ensure self-sealing bungs are fitted to each access point
- Use “octopus” connectors when connecting 2 or more compatible infusions to a single lumen
Toxic injection (local anaesthesia; cleaning fluid)
- Consider a closed system for saline flushes: 100ml bag 0.9% saline with a blunt fill needle inserted.
- Use a sealed chlorhexidine stick
Needle stick
- Use blunt needles for saline and local anaesthetic syringe loading
- Consider using a stitch set rather than handheld needle for suturing
- Reduce distraction to allow focus when handling sharps
- Safe, timely disposal of sharps into nearby sharps bin
Suturing
- Use a line of appropriate length
- If forced to use a longer than ideal line, ensure that the line itself is sutured to the skin not just the clips i.e. will need 4 sutures for correct fixation
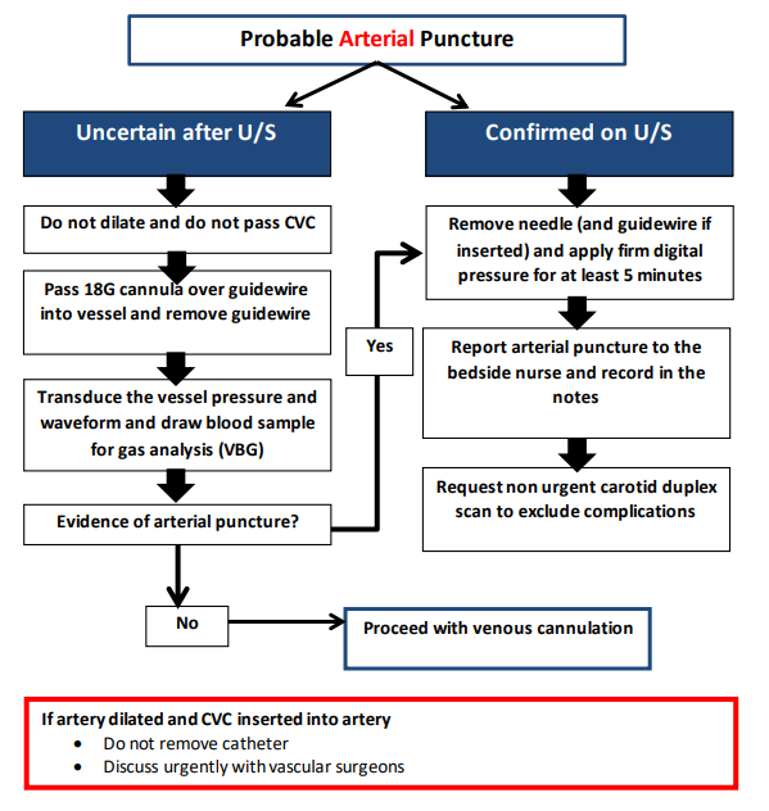
Arterial puncture
- Use real time ultrasound guidance to ensure correct vessel puncture
- Confirm guidewire position in vein with US before dilation
- Transduce proximal port and take VBG to confirm venous placement before use
- If concern re arterial puncture follow plan:
Retained guidewire
- Retain view of + / - hands-on guidewire during the procedure
- Guidewire should be removed before attempting aspiration or flushing of any ports on an inserted line.
- Do not allow distraction when exchanging the catheter over the guidewire
- Confirm guidewire removal with “WIRE OUT” declaration by operator and “WIRE OUT” acknowledgement from assistant
Post procedure CXR
- Confirm date, time and patient ID
- Review for pneumothorax, haemothorax, enlarged cardiac outline, line position
- Tip of CVC should be within the superior vena cava, just superior to the right atrium radiologically at the origin of the right main bronchus
- When inserting from the left side, the tip should not be abutting the side wall of the SVC
- Document the line depth at the skin at the time of the CXR.
