This diagram shows the organs involved in your digestive system. The small intestine and large intestine together make up what we call the "bowel".
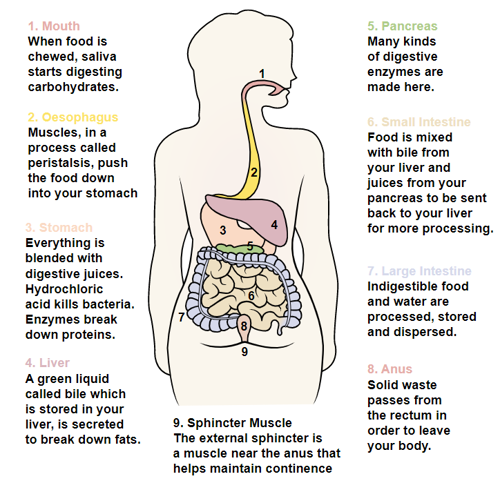

This diagram shows the organs involved in your digestive system. The small intestine and large intestine together make up what we call the "bowel".
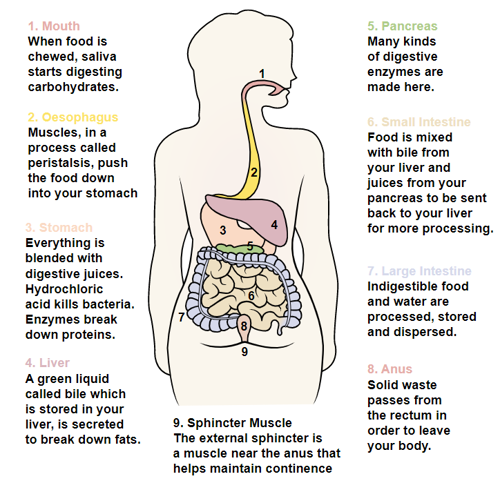
The bowel is part of your digestive system, whose role is to break down what you eat and drink. After a meal is digested, peristalsis (an involuntary muscle movement) pushes chewed food through the digestive tract.
Peristalsis takes place several times each day, most frequently after meals. This movement takes place without any input from the brain or spinal cord and is not affected by your spinal injury. As the bowel fills with stool it stretches, triggering messages to bowel muscles to move the stool down to the end of the large bowel and the rectum. When it is socially convenient, we will control our abdominal and pelvic muscles to allow us to empty the rectum to pass a motion. This is called a bowel movement.
The contraction of the abdominal muscles that assist with bowel activity, are controlled by nerves leaving the spinal cord at T6-T12. The lower end of the bowel is controlled by nerves leaving the spinal cord lower down at level S3-S5 (sacral vertebrae).
Some automatic (autonomic) control occurs within the bowel itself; this is the part that brings the urge to use the toilet when stressed or frightened.
After a spinal cord injury, the messages sent by the nerves located in your bowel are not able to reach your brain as before. This means you will not get the message that tells you when your bowel is full.
You may also lose control of the muscle at the opening from your back passage (sphincter). Your degree of loss will depend upon your level of injury and the extent (completeness) of your spinal injury.
It is important to remember that it can take a while for a bowel routine to become established. Once discharged, it is up to you and your healthcare provider to recognise when to adjust your bowel medications. You will learn how to do this during your rehab journey.
If your spinal cord injury is above T12, you will lose the control you normally had from your brain. However, you will be able to empty your bowel by stimulation – either through taking suppositories or by stimulating the bowel with your fingers.
With this type of injury, the message telling you that the bowel is full is not received and the muscle controlling the opening and closing of the anus stays tight. When the bowel gets full it empties automatically. This is called an upper motor neurone type bowel or reflex bowel.
If the injury is at or below T12, your bowel will not fully empty, even when stimulated. This is because the damage to the cord has damaged the pathways from the bowel wall into the reflex centre in the spinal cord. Therefore, there cannot be any reflex action.
This means that the bowel muscles will not squeeze, and the anal sphincter muscle remains relaxed. This is called a lower motor neurone type bowel or flaccid hypotonic bowel.
If your injury is incomplete or is around T12, you may find that your bowel can take on mixed upper and lower motor neurone type functioning.
If this is the case, you and the nursing team will work together to find a suitable management plan for your bowel.
The aim of a bowel routine is to allow your bowel to empty at regular intervals, e.g. daily, alternate days, in the morning or at night. We can time your bowel movement to suit you and consider your lifestyle, care needs etc. The two most important components of a good bowel routine are diet and timing.
How often you empty your bowels and your stool consistency is linked to the quantity and quality of food and drink you consume. A healthy diet including fibre in the form of bran cereals, fruits and vegetables can help keep the digestive process working.
Foods high in fibre can absorb and retain liquid and make the stool softer and easier to pass. Be aware of which foods work for you and which foods do not. For example, some vegetables are gas forming and could prove embarrassing. Also, some foods, alcohol and medicines can alter stool consistency and make bowel movements difficult. Food and drink that affected your stool consistency before your injury will still affect it. Make sure you take 2-3 litres of fluid each day to keep your stool soft.
A good way to understand and learn how different foods affect your bowel is to keep a food record. For about three weeks, write down what you eat and drink each day and describe your bowel movements. ‘ Bowel movements are often categorised by the ![]() Bristol Stool Chart.
Bristol Stool Chart.
Foods like coffee, tea, cocoa, or soft drinks contain caffeine which is a diuretic that may move the fluid out of your body. In fact, diuretics can cause you to lose more fluid than you drink. There is some evidence that caffeine stimulates peristalsis in some people. You may want to avoid drinking caffeinated drinks or limit how much caffeine you drink.
Alcohol affects bowel function. It can change bowel habits and reduce appetite, making it hard to stick with the diet part of your bowel routine. It can cause problems with continence and bloating. It may hinder your ability to cope and keep your routine regular. If you are having trouble following your bowel routine because of alcohol use, please tell your healthcare professional so they can help you.
It is important to do your bowel routine around the same time every day or alternate day. It can take several weeks to establish a good routine. If things are not going right do not be tempted to change after a few days or even a week. You should choose a time when you will not be rushing to complete your routine. Bowels empty more easily 30-60 minutes after a meal or warm drink (when the gastrocolic reflex is stimulated). You can time your routine to take this reflex into account to help you have a bowel movement. Once your routine is established, stick to it. The bowel is a creature of habit, and you may have ‘accidents’ if you change your routine frequently or change more than one part of your routine at a time.
When you can sit for four hours or more in your wheelchair, we will encourage you to get up to the toilet using a shower chair. Gravity helps move the stool down into the rectum. Check your skin regularly as some shower chairs or commodes can be be much firmer than your cushioned wheelchair. If you cannot use a shower for whatever reason, you can do your bowel routine in bed.
Physical exercise stimulates bowel function. The more active you are, the easier it is for the food to pass through the digestive system. Conversely you may find your bowel slows down if you are on bedrest for a period, if this is the case then you may need to increase your bowel medication.
There is some evidence that smoking directly affects colonic function. It is thought that nicotine can stimulate peristalsis in some occasional smokers and decrease it in some habitual smokers. For these reasons (and many others), you should consider stopping smoking. We have access to smoking cessation services to support you with this:
Aim for soft, formed stool that you can pass easily with minimal rectal stimulation. The bowel routine usually starts with digital stimulation or a stimulant medication, e.g. suppositories or enema. Digital stimulation involves inserting a lubricated gloved finger into the rectum and gently rotating it against the sphincter wall.
Aim for firm, formed stool that can be removed manually with ease and does not pass accidentally between bowel routines. Bowel care does not usually need chemical stimulants because the response would be very sluggish. People with a flaccid bowel should perform a manual evacuation.
Manual evacuation aims to empty the rectum with the fingers, this is usually described as ’the digital removal of faeces ‘. This procedure can be carried out either on the bed, showerchair or toilet. We will teach you how to do this. If you do this in bed it is better to lie on the side that leaves your dominant hand free with your uppermost knee bent up slightly and resting over your lower leg.
A colostomy is an operation to divert one end of the colon (part of the bowel) through an opening in the tummy. The opening is called a stoma. A pouch is placed over the stoma to collect your stool. A colostomy can be permanent or temporary.
Getting a colostomy is a personal choice and one which will be considered with consultation from your consultant. For some patients who find they are not in control of their bowel and their bowel is affecting the quality of their life then this may be an appropriate choice. Many patients who get this procedure say that they wish they had done it years ago. It is not for everyone however and may be something you consider many years following your injury.
Whilst in the spinal unit the staff and you will keep a record of your bowel activity using the bowel chart. The bowel chart records:
Once home you may choose to keep a diary of your bowel movements to establish a good routine. Often once discharged to your own home environment where you are eating homemade meals your bowel routine changes. The diary also allows you to track how different things affect your bowel.
NHSGGC Bowel Diary: ![]() nhsggc-bristol-stool-chart.pdf
nhsggc-bristol-stool-chart.pdf
If you ever find yourself admitted to another hospital it is important that you can direct your own care. Not all healthcare professionals are familiar with how to carry out bowel management. You may experience reluctance, or staff may even refuse to carry out manual evacuation claiming it is illegal.
You must explain that this procedure is not illegal and suggest that they should consult the Nursing and Midwifery Council for Nursing "Professional Code of Conduct" or the Royal College of Nursing document entitled "Management of Lower Bowel Dysfunction". You can also contact your Spinal Liaison Nurse or Education Nurse who can offer advice and educational support and training.
Should there be a suggestion that manual evacuation is not required then you should ask them to consult your GP (General Practitioner) or liaise with the spinal injuries unit. Manual evacuation is an essential part of your care and should not be omitted. You should explain to them that inappropriate adjustment or avoidance of your established bowel management programme can have serious consequences for your health and lifestyle. It is always useful to have a copy of your liaison nurse’s phone number to hand and the ward phone number for anything out of hours.
These are taken orally and increase bowel contractions. We often use these in the initial stages of the bowel programme. You should take these drugs eight to ten hours before you want to empty your bowels.
| Senna | Two tablets on alternate days or 10mls of syrup |
| Bisacodyl | 10mgs on alternate days (two tablets) |
Taken orally these are substances which are undigested and absorb fluid thereby increasing bulk and making the faeces soft. For example:
| Lactulose | 10 -15mls once or twice each day |
| Fybogel | One sachet every day |
| Bran | As instructed |
| Benefiber | As instructed |
These are inserted into the rectum and stimulate the reflex action of the bowel. For example:
N.B. You should not use large volume enemas regularly as they overstretch the bowel, causing it to lose its tone.
Osmotic laxatives work by drawing water into the stool to make it softer and easier to pass.
For constipation, take 2-3 sachets daily in divided doses. Only take 1 sachet at a time to see if it helps. You can take this for up to 2 weeks.
For faecal impaction– you can take up to 8 sachets per day, for up to 3 days.
You should dissolve each sachet in 125mls water. You can add juice to sweeten the taste.
This is a tear in the tissue around the anus as a result of passing hard stools or damage to the bowel lining caused by rough manual stimulation. These can be extremely painful and can cause an increase in spasm and even autonomic dysreflexia.
If you do not empty your bowel for a long time, the faeces become hard, dry, and more difficult to move (impacted). The symptoms are headaches, feeling sick and feeling full up, not being able to empty the bowel, sweating, increase in spasm, loss of appetite, and sometimes a brown, watery discharge from the anus. This can be caused by a change of diet and routine, low fluid intake, not eating and some drugs such as painkillers, antibiotics, and anti-depressants.
With chronic constipation, the bowel is blocked but some liquid may manage to leek past the blockage. This is often mistaken as diarrhoea. This condition is often called ‘overflow’ and should be treated right away.
If you suspect constipation then increase your fluid intake. If on an alternate day bowel routine then change to a daily routine until cleared double your senna and lactulose and consider introducing movicol.
These are varicose veins around or just inside the anus. You may be prone to developing these because of a lack of mobility and poor circulation. They are caused or made worse by straining for long periods on the toilet and by rough manual evacuation. If the haemorrhoids are bad, it will complicate the process of bowel management, and can bring on autonomic dysreflexia in tetraplegia or high paraplegia patients. Haemorrhoids may also cause rectal bleeding. You should discuss these with your GP or liaison nurse. Surgery may be necessary but there are other treatments that you can try first e.g. haemorrhoid creams.
This is an unformed, loose stool which may cause unplanned bowel movements or "accidents". It can cause discomfort, often in the form of abdominal cramps. Diarrhoea can also lead to skin breakdown through faecal burning of the skin by the liquid stool. You may have to stop taking any laxatives until diarrhoea clears up. You may also have to put yourself on bed rest to try and reduce any skin breakdown from sitting in wet, soiled clothing.
This is just as embarrassing now as it was before your injury. The odour will depend on what you have eaten. Your wind will smell bad after you eat food that is high in protein, such as meat, fish, or eggs. If you eat a vegetarian diet, your gas probably won’t smell as bad, but you will have a lot of it.
You may experience bloating due to excessive bacterial breakdown of bowel contents, for example intolerance to dairy products (lactose intolerance). Please discuss this with your GP as medications can help.
To help avoid this issue you may wish to consider the following points:
You should also think about how you eat. Excessive gas may be due to swallowing excessive air while you are eating or drinking. Eat your food slowly, chew with your mouth closed, try not to gulp your food, and do not talk with food in your mouth.
Be aware of foods that can cause gas try to avoid specific foods from your diet. You can remove foods one at a time until you have learned which (if any) cause you to have gas, and then cut down on those foods.
Checking your bowel programme and increasing the frequency of bowel care may reduce the amount of stool you store in your colon that will produce gas. Do not try too hard to hold in the gas as this can give you a stomachache or headache.
Remember: Passing wind means your digestive system is working. It was ok to pass wind before your injury; it is still ok to pass wind now!
![]() It took me a long time to get a bowel routine established while I was in hospital. It was one of the most difficult things about my rehab but once established I have had very few problems since.
It took me a long time to get a bowel routine established while I was in hospital. It was one of the most difficult things about my rehab but once established I have had very few problems since. ![]()