Skin tolerance is the length of time you can lie or sit on one area without getting a red mark. Everyone’s skin tolerance is different. It is important to know what your skin tolerance is.
If lying or sitting on a different surface than usual, your skin tolerance time may be different so if you are trying a new surface for the first time, check your skin more frequently.
How often should the skin be checked?
Whilst in hospital specialist spinal nurses will check your skin and encourage you to check your own skin every time you change position in bed and every time you get up and on return to bed. This is to establish what your skin tolerance is.
This is the policy followed in the spinal injuries unit to build up your skin tolerance:-
- Everyone commence turning at 2 hourly intervals – side/side turns should be encouraged to ensure the sacral and buttock areas are kept free from pressure and allow reperfusion whilst in bed. These areas are more prone to pressure damage when in your wheelchair.
- If each hip/side remains free from pressure damage after 2 hourly turns, turns can be increased to 3 hourly side/side.
- If each hip remains free from pressure damage after 3 hourly turns, turns can be increased to 4 hourly side/side.
- Once turning 4 hourly side/ side is achieved the following steps are taken:
-
- 4 hourly side/side turns – repeat this twice, and if the skin remains free of pressure damage progress to -
- 5 hourly side / side turns - repeat this twice, and if the skin remains free of pressure damage progress to -
- 6 hourly side / side turns - repeat this twice, and if the skin remains free of pressure damage progress to -
- 7 hourly side / side turns - repeat this twice and if the skin remains free of pressure damage progress to -
- 8 hourly side / side turns - repeat this twice and if the skin remains free of pressure damage increase until 10 hourly side / side turns are achieved.
The aim is to achieve turn times twice, on each side, with no pressure damage occurring. Turn times will only be increased as above when the skin remains intact, showing no signs of pressure damage at all.
For example, if you are in your wheelchair during the day it will take 4 nights to achieve 8 hourly turns safely. If positioned on the right side on night 1 for 8 hours, then on night 2 you will be positioned on the left side, and this would be repeated for night 3 and 4. This approach allows skin tolerance to be built up safely. If any damage is noted at all then you should not be positioned on the side with damage until the damage has resolved. You will will have to incorporate time on your back whilst sleeping.
Following this process allows you to have the confidence to sleep in the same position without the need to be turned overnight. Which not only leads to a broken nights sleep but also potential need for carers coming into your home.
By the time you go home you should know what your skin tolerance is. Routinely you should check your skin twice a day:
- Once before getting up in the morning
- Once before going to bed at night
However, if you have any skin problems you need to check your skin more often. Any broken, red or bruised areas need to be kept totally pressure free until they heal completely.
How do I position myself in bed?
If your skin tolerance is 8 hours that means you should turn every 8 hours. If it is 6 hours then you should turn every 6 hours etc.
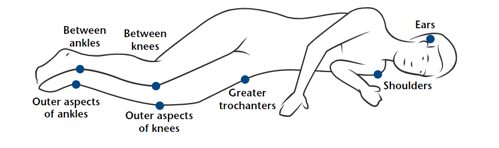
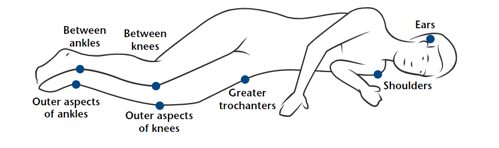
When lying on your side, the risk areas are:


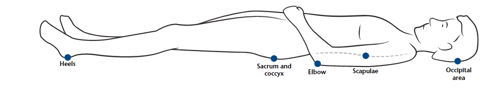
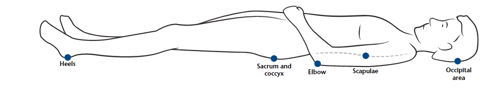
When lying on your back, the risk areas are:


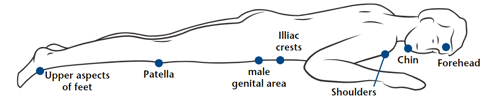
When lying face down, the risk areas are:
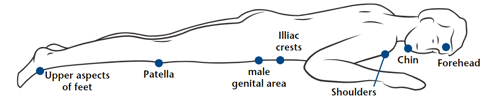
Using pillows at risk areas can help in relieving pressure. Lying face down is also good for straightening your hips and knees and can reduce leg spasms.
How can I relieve pressure in my wheelchair?
When sitting in your chair, it is important that you relieve pressure regularly. You can do this in a number of ways.
Lifting buttocks from chair
In order to do this you need to have good arm strength. Apply brakes and push up either from the armrests or wheels until your buttocks are free of the chair. Count to 20 slowly and then come back down again. Do this every 15 minutes.


Leaning from side to side
If you do not have good arm strength then going from side to side is an alternative. Apply brakes, hook your arm around back of chair and then lean to opposite side that takes the pressure off that side of the buttock. Count to 20 slowly and repeat on the other side.




Tilting forward
Tilting forward is another effective method but again you need good arm and balance control unless there is someone to help you. Apply brakes, bend forward (moving your chest towards your knees), balancing by leaning your arms on your upper thighs or wheelchair. This lifts the weight of the buttocks off the chair seat.


When do I need bed rest?
If a red mark develops over your hips, buttocks, or lower back, stay off the affected area. This means staying in bed until it the damage has resolved. If the pressure damage is caught early and fades within 30 minutes the time spent on that side should remain static until skin tolerance is achieved. If pressure damage takes more than 30 minutes to fade, you should not lie on that side. If tissue damage does not fade, for example, if there is a red area on the left hip then then you should only lie on the right side and the back.
Whilst in the spinal unit, if pressure damage is unresolved then a therapy mattress would be requested. Turns onto the unaffected pressure areas do not need to be reduced to 2 hourly because a therapy mattress has a higher pressure relieving property than a normal mattress. When home you may already have a therapy mattress. If not you can contact your district nurse to have one ordered for home delivery or you may be offered an overlay mattress with greater pressure relieving properties than your current mattress.
Turn times on a therapy mattress should be reduced by half of what they were. For example, if someone has pressure damage on the left side and was turning 8 hourly, turns would be changed to 4 hourly right side and back with the left side remaining pressure free.
When the pressure damage has healed and 8 hourly skin tolerance has been achieved on a therapy mattress, you would be transferred onto a foam mattress. Turns are then reduced to 2 hourly and built up as before in steps 1-4 of building skin tolerance up whilst in bed. Intervals between turns should always be reduced to 2 hourly when changing from a mattress with greater pressure relieving properties to one with lesser pressure relieving properties.
What do I do when skin has healed?
If there has been a skin problem requiring a period of rest in bed then once it has completely healed you can gradually get up. If you are in any doubt please contact your spinal liaison nurse for guidance on how to manage this process safely and effectively without compromising your skin.
Guidelines for mobilisation (getting up) following bed rest
When your pressure areas have completely healed you can begin the process of mobilising in your wheelchair again. We take this slowly accessing the pressure areas on return to bed and prior to mobilising.
The following is a guide to mobilising following a period of bedrest:-
- When mobilising following a period of bed rest for pressure damage and you have been on bedrest for 2 days or less, no change is required to your sitting time (if the cause has been alleviated, consider cushions clothing etc). If you have been on bedrest for 7 days or less, the sitting time is reduced to 1 hour and built up by 30 minutes per day. If you have been on bed rest for 8 days or more, then you should start mobilising for 15 mins sessions only.
- If you have been on bedrest for a non-pressure related problem, for example you have had the flu an infection or problems with your bowels, and have been on bedrest for 2 days or less, no change is required to your sitting time. If they have been on bed rest for 7 days or less your sitting time is halved and increased by 1 hour per day. If they have been on bedrest for 8 days or more, the sitting time starts at 1 hour and is increased by 30 minutes per day. If you have been on bed rest for 2 weeks or more, you should start sitting up for 30 minutes.
Review you pressure areas before mobilising and on return to bed.
| Day 1 |
Up for 15 mins x 2 |
| Day 2 |
Up for 30 mins x 2 |
| Day 3 |
Up for 45 mins x 2 |
| Day 4 |
Up for 1 hr x 2 |
| Day 5 |
Up for 1 hr 30 mins x 2 |
| Day 6 |
Up for 2 hrs x 2 |
| Day 7 |
Up for 2 hrs 30 mins x 2 |
| Day 8 |
Up for 3 hrs x 2 |
| Day 9 |
Up for 3 hrs 30 mins x 2 |
| Day 10 |
Up for 4hrs x 2 |
Once you get to four hours twice daily you may find it easier to have one session sitting in the middle of the day e.g.
| Day 11 |
Up for 4hrs 30 mins x 1 |
| Day 12 |
Up for 4hrs 30 mins x 1 |
| Day 13 |
Up for 5hrs x 1 |
| Day 14 |
Up for 5hrs x 1 |
| Day 15 |
Up for 5hrs 30 mins x 1 |
| Day 16 |
Up for 5hrs 30 mins x 1 |
| Day 17 |
Up for 6hrs x 1 |
| Day 18 |
Up for 6hrs x 1 |
| Day 19 |
Up for 7hrs x1 |
| Day 20 |
Up for 7hrs x1 |
| Day 21 |
Up for 8hrs x1 |
| Day 22 |
Up for 8hrs x1 |
- Check your pressure areas every morning and every night!
- Use or a mirror or take a picture using your mobile phone for areas that you can’t be seen.
- Take action immediately! When you detect a red mark or even suspect pressure damage is forming and sitting in your wheelchair will put pressure on the area of concern, go onto bed rest and ensure the affected area remains pressure free. You can then mobilise when resolved.
- Whilst in the spinal unit you will be supported with decision making regarding pressure area care. Once discharged if you have any concerns please contact your spinal liaison nurse or district nurse for advice.